This device delivers magnetic pulse to the head at touch of a button. Scientists say handheld device can alleviate symptoms for up to two hours. Treatment relieved or reduced excruciating pain in 73 per cent of patients taking part in trial
What is Migraine?
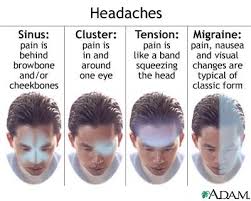
The pain of a migraine headache is often described as an intense pulsing or throbbing pain in one area of the head. However, it is much more; the International Headache Society diagnoses a migraine by its pain and number of attacks (at least 5, lasting 4-72 hours if untreated), and additional symptoms including nausea and/or vomiting, or sensitivity to both light and sound.
Some facts about Migraine

Migraine is three times more common in women than in men and affects more than 10 percent of people worldwide.
Roughly one-third of affected individuals can predict the onset of a migraine because it is preceded by an "aura," visual disturbances that appear as flashing lights, zig-zag lines or a temporary loss of vision.
People with migraine tend to have recurring attacks triggered by a number of different factors, including stress, anxiety, hormonal changes, bright or flashing lights, lack of food or sleep, and dietary substances.
Migraine in some women may relate to changes in hormones and hormonal levels during their menstrual cycle. For many years, scientists believed that migraines were linked to the dilation and constriction of blood vessels in the head. Investigators now believe that migraine has a genetic cause
Is there any treatment?
There is no absolute cure for migraine since its pathophysiology has yet to be fully understood. There are two ways to approach the treatment of migraine headache with drugs: prevent the attacks, or relieve the symptoms during the attacks. Prevention involves the use of medications and behavioral changes. Drugs originally developed for epilepsy, depression, or high blood pressure to prevent future attacks have been shown to be extremely effective in treating migraine. Botulinum toxin A has been shown to be effective in prevention of chronic migraine. Behaviorally, stress management strategies, such as exercise, relaxation techniques, biofeedback mechanisms, and other therapies designed to limit daily discomfort, may reduce the number and severity of migraine attacks. Making a log of personal triggers of migraine can also provide useful information for trigger-avoiding lifestyle changes, including dietary considerations, eating regularly scheduled meals with adequate hydration, stopping certain medications, and establishing a consistent sleep schedule. Hormone therapy may help some women whose migraines seem to be linked to their menstrual cycle. A weight loss program is recommended for obese individuals with migraine.

What is the prognosis?
Responsive prevention and treatment of migraine is incredibly important. Evidence shows an increased sensitivity after each successive attack, eventually leading to chronic daily migraine in some individuals With proper combination of drugs for prevention and treatment of migraine attacks most individuals can overcome much of the discomfort from this debilitating disorder. Women whose migraine attacks occur in association with their menstrual cycle are likely to have fewer attacks and milder symptoms after menopause.
What research is being done?
Researchers believe that migraine is the result of fundamental neurological abnormalities caused by genetic mutations at work in the brain. New models are aiding scientists in studying the basic science involved in the biological cascade, genetic components and mechanisms of migraine. Understanding the causes of migraine as well as the events that effect them will give researchers the opportunity to develop and test drugs that could be more targeted to preventing or interrupting attacks entirely. Therapies currently being tested for their effectiveness in treating migraine include magnesium, coenzyme Q10, vitamin B12, riboflavin, fever-few, and butterbur.
In 2010, a team of researchers found a common mutation in the gene TRESK which contains instructions for a certain potassium ion channel. Potassium channels are important for keeping a nerve cell at rest and mutations in them can lead to overactive cells that respond to much lower levels of pain. Large genetic analyses similar to the one used to identify TRESK will most likely lead to the identification of a number of other genes linked to migraine.
New Device- Migraine Sufferers Find Relief from Handheld Magnetic Device

A handheld magnetic device may be a way for migraine sufferers to take treatment into their own hands. At a congress last week, researchers revealed how three months of treatment with the device relieved or reduced headache pain in 73% of patients treated. Headache specialists at several clinics around the UK, including in Aberdeen, Bath, Exeter, Hull, Liverpool and London, are prescribing the non-invasive single pulse Spring Transcranial Magnetic Stimulation (TMS) device, made by eNeura Technology in California. The new data, from a trial involving 60 migraine sufferers treated with TMS at UK clinics, was presented at the 3rd European Headache and Migraine Trust International Congress in London on Friday. The news comes in the wake of a warning by the National Institute for Health and Clinical Excellence (NICE) in England and Wales, that painkiller overuse can cause headaches.
The TMS device costs about £500 and is about the size and weight of a portable radio. As soon as he or she senses a migraine coming on, the user holds it to the back of the head and pushes a button. This sends a brief magnetic pulse into the brain. Scientists suggest that magnetic pulses could halt migraines before they get the chance to build. Scientists believe the magnetic pulse somehow short-circuits the electrical storm that builds up at the start of migraine headaches. The congress also heard how the TMS improved other symptoms of migraine in 63% of the trial participants: symptoms such as vertigo, nausea, memory problems, and hyper-sensitivity to light and noise.

And over half (53%) reported a reduction in the number of headache days.
Andy Bloor took part in the UK trials. He suffers from chronic migraines and says the TMS device worked for him, “The key for me was using the device quickly - as soon as the migraine started. He says when he did that, the migraine stopped. "The plus of the device is it reduces my reliance on strong drugs like cocodamol," he adds, in a report on the congress by the UK Press Association. Findings from a trial of the efficacy of the TMS device were published in The Lancet Neurology in 2010. They say the device offers efficient pain relief for up to 48 hours after treatment in some patients with migraine with aura, and does not cause any serious side-effects.
Professor and neurologist Peter Goadsby, one of the world's leading headache experts and researchers, was joint chair of the London congress. He told the press, “For the many migraine sufferers whose medicines just do not do the job, it is exciting to see such an innovative, novel approach to treatment that provides new optimism.
Although TMS is often regarded as safe, the greatest acute risk of TMS is the rare occurrence of induced seizures and syncope…. Besides seizures, other risks include fainting, minor pains such as headache or local discomfort, minor cognitive changes and psychiatric symptoms (particularly a low risk of mania in depressed patients.
What is eNeura sTMS Technology?
Transcranial Magnetic Stimulation
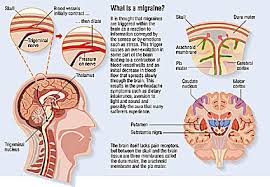
Migraine is often described as an electrical storm, in which the brain is hyperexcitable with an abnormal response to normal stimuli or triggers. The result can be an excruciatingly painful headache. Clinical research has shown that a brief pulse of energy, such as transcranial magnetic stimulation (TMS), may be effective in interrupting or short-circuiting the progression of migraine.
TMS Technology
TMS technology has been used for many years to study the brain. The most robust and widely accepted use is in measuring the connection between the primary motor cortex and muscles. This is most useful in monitoring stroke, spinal cord injury, multiple sclerosis and motor neuron disease. TMS is based on the principles of induction—rapidly changing magnetic fields that induce electrical currents. When TMS is applied to the back of the head, a magnetic field of very short duration passes through the skull and tissue non-invasively and without discomfort. The magnetic field induces very mild electrical currents in the brain tissue to excite and depolarize neurons in the brain. This process is thought to interrupt the abnormal electrical activity associated with migraine and cortical spreading depression (CSD).
eNeura sTMS Technology
eNeura technology utilizes single-pulse Transcranial Magnetic Stimulation, or sTMS. The SpringTMS™ Total Migraine System delivers each treatment in a millisecond (1/1,000 of a second). By comparison, a typical magnetic resonance imaging (MRI) device continuously delivers a magnetic field that is more than twice as strong, and with each session lasting more than 20 minutes. Two decades of clinical experience with sTMS has consistently demonstrated it to be a non-significant risk technology, with promise in the diagnosis, monitoring and treatment of neurological and psychiatric disease in adults.1-3
(Source- 3rd European Headache and Migraine Trust International Congress in London)
No comments:
Post a Comment